What’s Paris got to do with it?
Subtitle: O.G. medicine’s origin story and how to optimize healthcare like a Parisian restaurant
By Olivia Geen, MD, MSc, FRCPC
| 8 min read |
I am a doctor-meets-travel-writer who explores topics in healthcare using real-life adventures in medicine and abroad.
It all began in Paris. It’s probably not unusual to have an existential crisis in a city like this; big experiences bring big insights, and this city is full of them.
I was just visiting for 2 days - a short trip at the end of a 6-week stay at Oxford, where I was working on my Master’s in Translational Health Sciences.
It was there, one night in Paris, that I had an idea. The idea became this blog post, and this blog post became the foundation for OG Medicine.
As you’ll discover on my About page, this website pulls together ideas in healthcare, innovation, wellness, philosophy, style and travel, using experiences from my own life, tailored for people like you, who work or are interested in healthcare.
Whether it’s experiences from my work as a specialist physician in Canada, my previous role as a Clinical Scholar at McMaster University, my current master’s research at the University of Oxford, or my role as an advisor for healthcare startups, I write using both evidence and experience to bring you interesting insights and practical tips for a life in - and out - of medicine.
In a future post, I’ll explain my methods in more detail, but for now… here’s the origin story of OG medicine, written at midnight in Paris.
THE OG MEDICINE ORIGIN STORY
Tonight I went to a little restaurant called Le Chanard. It's only one minute away from the hotel that I am staying at, Charles V. After walking all over Paris, finding an authentic French chef right down the road was exactly what I needed.
The restaurant was small, with only 8 tables plus the bar, and like other local places, it had a daily menu written in chalk.
The waiter placed the menu board on the chair opposite me, and I quickly proceeded to google translate all the items on the list. J'apprend plus mots de Francais chaque jours, mais maintenant, mon Francais c'est mal.
The menu the night OG Medicine was born.
The food was incredible, and without it, OG Medicine might never have been born (or more realistically, born months later, instead of right there while sitting at the table). Because without the incredible food, I might not have sat there wondering how they planned such a perfect menu. I might have left quickly after eating, and not overheard the waiter tell the next table over that they were all out of a particular dish for the day (the dish that I had just finished eating).
I might not have felt comfortable to sit there longer, savouring my Tarte au Citron while I read a pocket book (my secret to eating dinner alone), and thinking to myself how much I longed to write myself. And it might not have occurred to me that the restaurant I was in was very similar to the Canadian healthcare system, and that we could learn a thing or two from them.
Thankfully all those things happened, and I ended up observing the process of optimization in a complex system; I realized that Le Chanard faced the same problems as healthcare.
Once I saw the similarities, ideas started to take shape. Finding parallels between two seemingly very different things has always helped me understand complex topics.
Whether it be human physiology (the immune system is an army with different types of warriors), diseases (frailty is like melting ice that can’t withstand much pressure), or technology (using an EMR is like deciding to get the new iPhone; do you need it, does it work well, and will you be ostracized if you stick with your Nokia flip phone).
I found myself wanting to share my quirky analogy with someone, thinking that it might help other people like me who work in healthcare yet often find themselves wondering how did we get here? what is going on? why do I still have a pager?
That’s when OG medicine was born.
On this website you’ll find articles that pull from all facets of my life - physician, researcher, innovator, advisor, traveler, and most of call, curious enthusiast for life itself.
The goal to bring you insights for your life in healthcare, sprinkled with the magic of travel, wellness, philosophy, and adventure.
In the end, perhaps together we might use these ideas to create a new system that works for us all.
Let’s start with an analogy in Paris.
Midnight on the Seine, where I started to write.
HOW TO OPTIMIZE HEALTHCARE LIKE A PARISIAN RESTAURANT
1) How are these things similar?
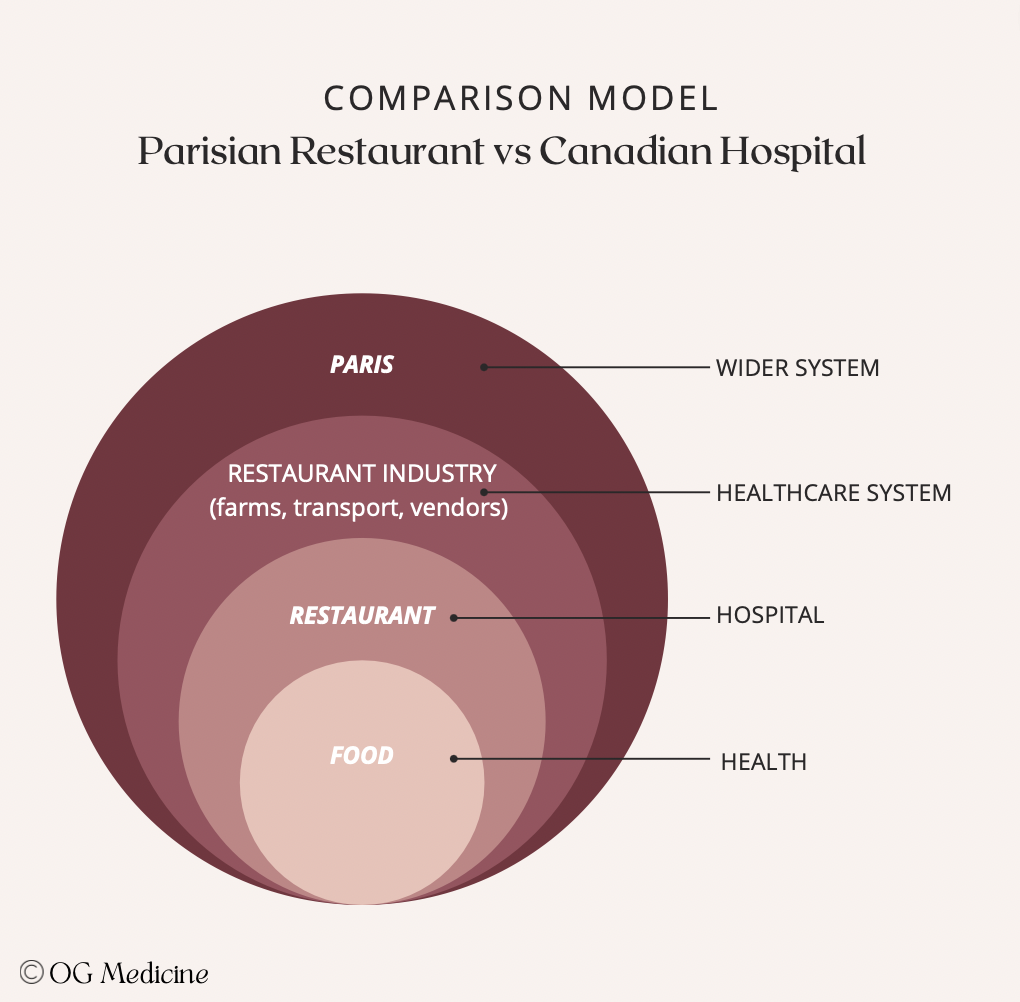
A Parisian restaurant, like a hospital, exists within a wider network - it can't operate in isolation.
In the case of Le Chanard, they need customers to sell the food to, the farmers and vendors to provide the raw ingredients, and the wider city of Paris to bring people into its radius. Many people are needed to populate each of these spheres in the ecosystem and interact with the restaurant throughout its existence. Customers, chefs, waiters, farmers, truck drivers, engineers, city workers, law-makers, and more.
In the case of a hospital, we find that it is very similar. It also exists in a wider network, where it needs patients to provide health to (health is essentially the product we provide), the pharmaceutical and industry partners to provide the raw ingredients (drugs and devices) and materials to sustain our services, and the wider city to have patients who go to the hospital. There are also many individual people at each of these spheres; from patients, to healthcare workers, to pharmaceutical reps and scientists, administrators, politicians, and more.
A Parisian restaurant and a hospital aren’t so different after all…
Thus, both a restaurant and a hospital are intrinsically and irrevocably linked to the smaller spheres - customers and patients - and the bigger spheres - the industry or system within which it sits. All of these spheres are constantly changing and evolving around the restaurant, which also changes and evolves as a result.
The question is - will they evolve together into a successful restaurant business? Or will one or more of the spheres disengage and cause the business to collapse?
2) How do restaurants succeed?
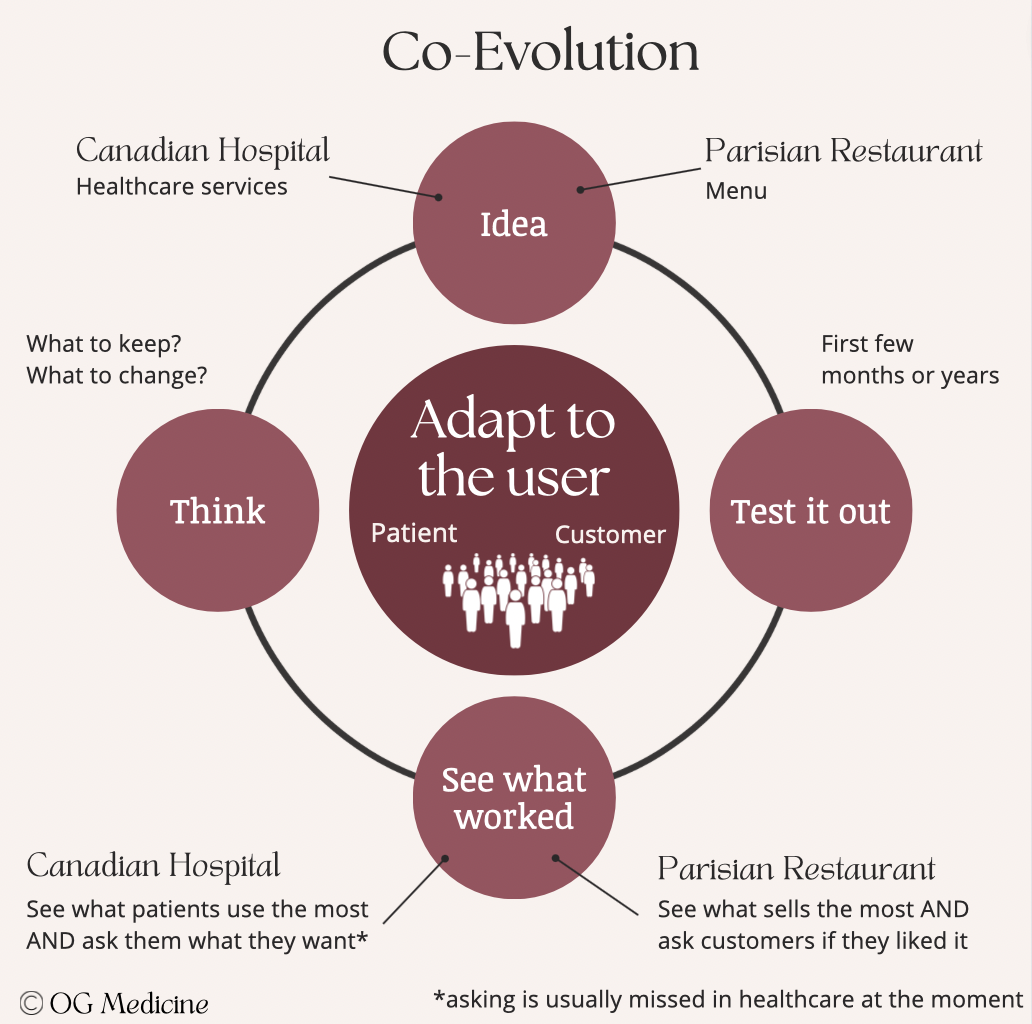
When a little Parisian restaurant first starts out, it guesses what its customers will like. The chef will undoubtably make some educated choices, pulling from past experience, friends and family, and perhaps even testing the menu out on a few "early adopters".
Once the restaurant opens, patterns will start to emerge from the customers. Crowd favourites will start to appear. This will mean buying more ingredients for the favourites, and less ingredients of the others, if the the restaurant is to keep costs low and reduce waste. The restaurant evolves based on what its customers need.
In healthcare, the same thing (almost) happens. When a new hospital opens, it makes a best guess of what the people in that area will need, using epidemiological data on health and disease. Over time, it gathers information on what conditions are seen the most in hospital, and adjusts its services accordingly.
Thus, in a complex system (with multiple layers of interacting people) the spheres will co-evolve over time. In the restaurant business, the larger spheres change to meet the needs of the smallest sphere; the customer. However, in healthcare, even though we all agree in principle that patients are the most important thing, in practice we often turn our focus to the bigger spheres.
This gets us into trouble, and can start to answer the question of how did we get here?
3) Why isn’t our healthcare system working?
Although disentangling all the details of the problem might seem impossible, there are actually only two fundamental causes for the mess that we’re in:
A) We don’t optimize for the smallest sphere:
If we adapt ourselves to a different sphere, let's say the wider political system, or the pharmaceutical industry, we don't necessarily end up with an inner sphere that matches what people want or need, because we weren't trying to. If we get lucky and we optimize health in the process, this is a happy accident, not the grand design.
If we want to optimize health, we need to adapt ourselves to what that sphere needs. It's a pretty simple concept really.
B) We don’t ask people what they want in the right way:
Unlike a Parisian restaurant, the hospital and healthcare system collect mostly numbers (or quantitative data) on how things are being used. We don't often ask patients "What do you actually want?".
As a result, we get a system that optimizes for what people are using, without understanding whether it’s what they actually want. Part of the challenge is that health itself is quite nebulous. What even is it? Just the absence of disease?
A more helpful definition that I use to guide my treatment plans with patients is the idea that health is the ability to move, think, and feel in whatever way seems right to you. While we can’t always keep health at 100% forever, there is a lot we can do to optimize the body (move), mind (think) and spirit (feel), which incidentally doesn't always mean living longer if it comes at the expense of who you are.
Thus, if we want to optimize for the smallest circle, we’ve got to ask the people there what they want, using creative and intelligent questions (not just numbers) to get at what they need. This moves beyond “patient-centered care” or “patient partners”.
It means fundamentally shifting our intentions to human-based care where we forget about the biomedical model of health as the absence of disease, and consider it as the presence of a full human life.
4) Great, now what?
One final message about complex systems is that they are made up of people in those spheres. We label things to group them together - “hospital”, “government”, “healthcare system” - but at the end of the day, those labels are just a collection of people that come together to make something new.
This is why the fundamental shift is to not think of problems as “how do we change the system”, but “how do we change the people in the system”.
I don’t mean this in the sense that the weight of the problems are on the shoulders of front-line healthcare workers alone (as is often implied when administrators tell us to do yoga to fix burnout).
I mean this in the sense that everything comes down to those spheres and what the people inside them decide to do, both at the “micro” (patient) level and the “macro” (government) level.
Government is still just a group of people sitting in meetings having conversations. What will they decide?
If we want to change the system, we have to change what people do. How? Well, we’ll dig into that in many posts here, but ultimately the most permanent way to change people is to change the high-level ideas that they follow.
Bonne nuit.
Olivia
Dr. Geen is an internist and geriatrician in Canada, working in a tertiary hospital serving over one million people. She also holds a masters in Translational Health Sciences from the University of Oxford, is widely published in over 10 academic journals, and advises digital healthcare startups on problem-solution fit and implementation. For more info, see About.
Influences:
1) Life experiences
2) Translational Health Sciences from the University of Oxford