How to Solve Problems in Healthcare
Subtitle: How to use complexity thinking to solve problems in healthcare
By Olivia Geen, MD, MSc, FRCPC
| 25 min read |
This article will tell you how to tackle any problem that you encounter in your quest to change the system.
There are a number of different fields that study the science of change and innovation in healthcare and the tricky challenge of getting those changes into the daily practice of medicine.
This includes fields like Implementation Science, Behavioural Sciences, Organizational Science, Knowledge Translation, and Translational Health Sciences.
They might go about it in different ways with different goals - implementing guidelines, new technologies, or services - but at the core, all fields aim to solve problems in healthcare by introducing new solutions that are used widely and well.
In this article I’ll introduce you to a new philosophical paradigm used in Translational Health Sciences, first encountered during my master’s at the University of Oxford. I’ve distilled the theoretical into 3 practical, evidence-and-experienced-based strategies that can be used to achieve your goals in healthcare.
At the end you’ll understand why success hinges on realizing that healthcare is not a machine; it’s a complex adaptive system.
Now sit back, relax, and learn how to solve healthcare in 3 parts:
Part 1: Evidence - recognizing healthcare as a complex adaptive system
Part 2: Explanation - what is a complex adaptive system
Part 3: Strategy - how to solve problems in healthcare using complexity
Feedback Loops - use feedback loops to eliminate problems
80/20 Rule - solve the 20% of causes that account for 80% of the problem
Effectual Logic - start with what you’ve got
Let’s begin.
PART 1: THE EVIDENCE
Recognizing healthcare as a complex adaptive system
If we want to change a system, we need to first understand what kind of system we’re dealing with, before we can ever hope to solve it.
It doesn’t take a genius to recognize the imperative of knowing what before how.
After all, you wouldn’t try and solve a Rubik's cube in the same way you solve a cross-word puzzle, would you? Of course not. If you want to solve the game, you’ve got to first recognize the specific game that you’re playing, before being able to identify the rules and secrets to winning.
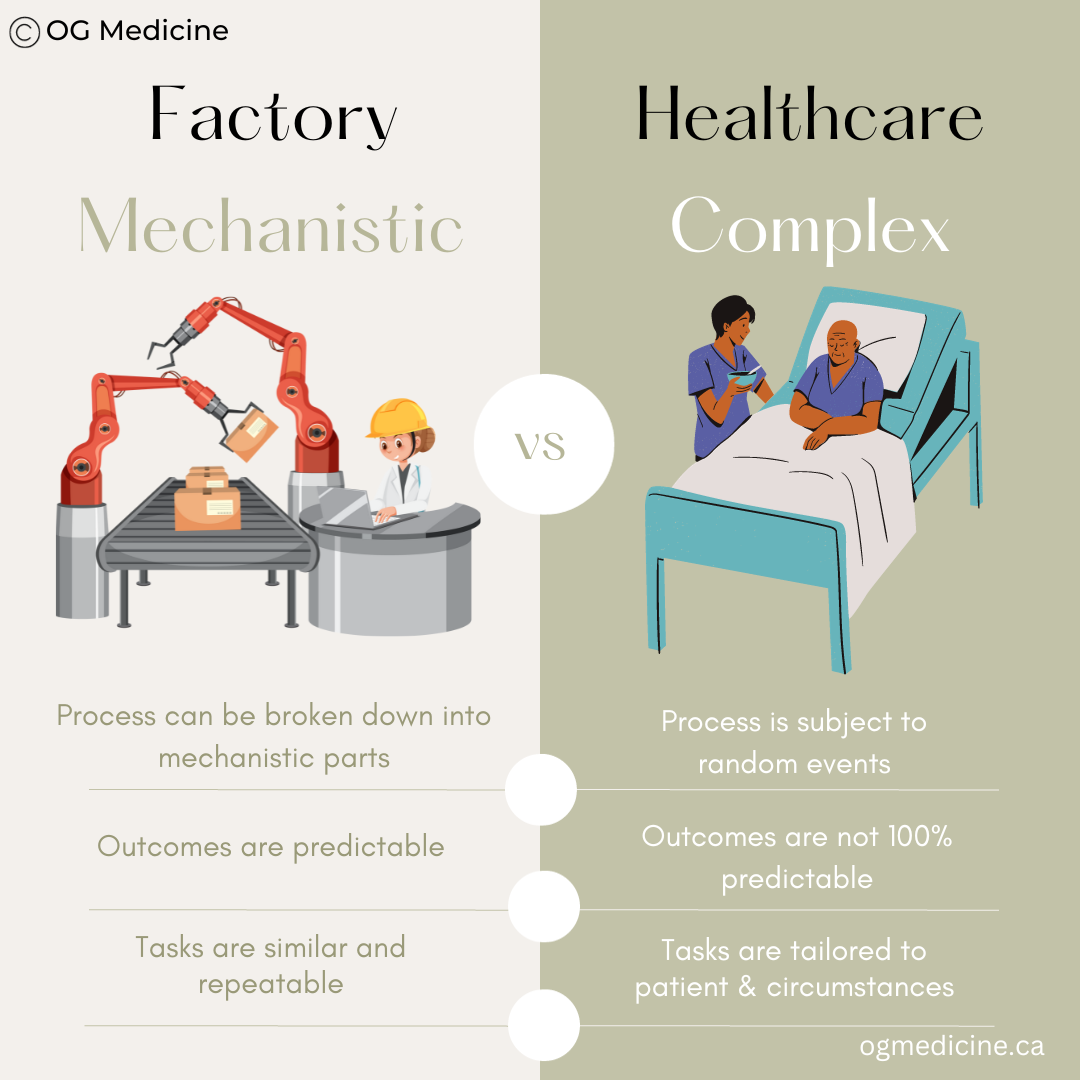
There are two dominate schools of thought when it comes to the (very serious) “game” of healthcare systems - mechanistic vs complex systems.
Mechanistic (complicated) thinking vs complexity thinking in healthcare.
The prevailing logic in healthcare design in the 1980s- early 2000’s was one of “machine-logic” - the idea that problems in healthcare could be broken down into discrete steps, improved in isolation, and then combined again to produce a superior product (i.e. health outcomes).
However, over the last 20 years, experts have come to understand healthcare as a complex adaptive system, in which there are constant dynamic changes, competing goals, unpredictable outcomes, and the need for care that is tailored to the individual patient, rather than cookie-cutter care-for-all (which ends up being care-for-no-one).
I was first introduced to the idea of complexity by Professor Trisha Greenhalgh, renowned researcher and physician at the University of Oxford. Once I understand the concept, I began to see evidence of complexity in everything I did back home as a doctor.
Thanks to Greenhalgh and many others, there is now an established and extensive evidence-base on complexity in healthcare that aims to guide systems-thinkers, doctors, policymakers, and innovators in decision-making and system-design. BMJ has a whole series; the WHO has released manuals and guides, and more and more papers are published every year.
Importantly, complexity isn’t unique to healthcare. Evidence of CAS across systems and society is mounting, and spans many disciplines - it’s talked about in economics (the stock market is a CAS); ecology (any animal or insect with a “hive mind” tends to form a CAS, like bees and ants); mathematics (non-Euclidean geometry and fractals); computer programming (neural networks and the natural language-processing underlying ChatGPT are all CAS); and the list could go on.
Suffice is to say - brilliant minds across continents and disciplines have published extensively on the evidence of complexity in our social systems and world, including in healthcare.
The rest of this article pulls together key concepts combined with my own insights from working in healthcare and advising healthcare startups (with entrepreneurship being a CAS of its own), into practical advice tailored to people working or interested in solving problems in medicine.
But first - just a little bit of the theoretical underpinnings so you can understand the strategic solutions presented in Part 3. In the next section we’ll tackle what exactly a complex adaptive system is.
PART 2: THE EXPLANATION
What is a complex adaptive system?
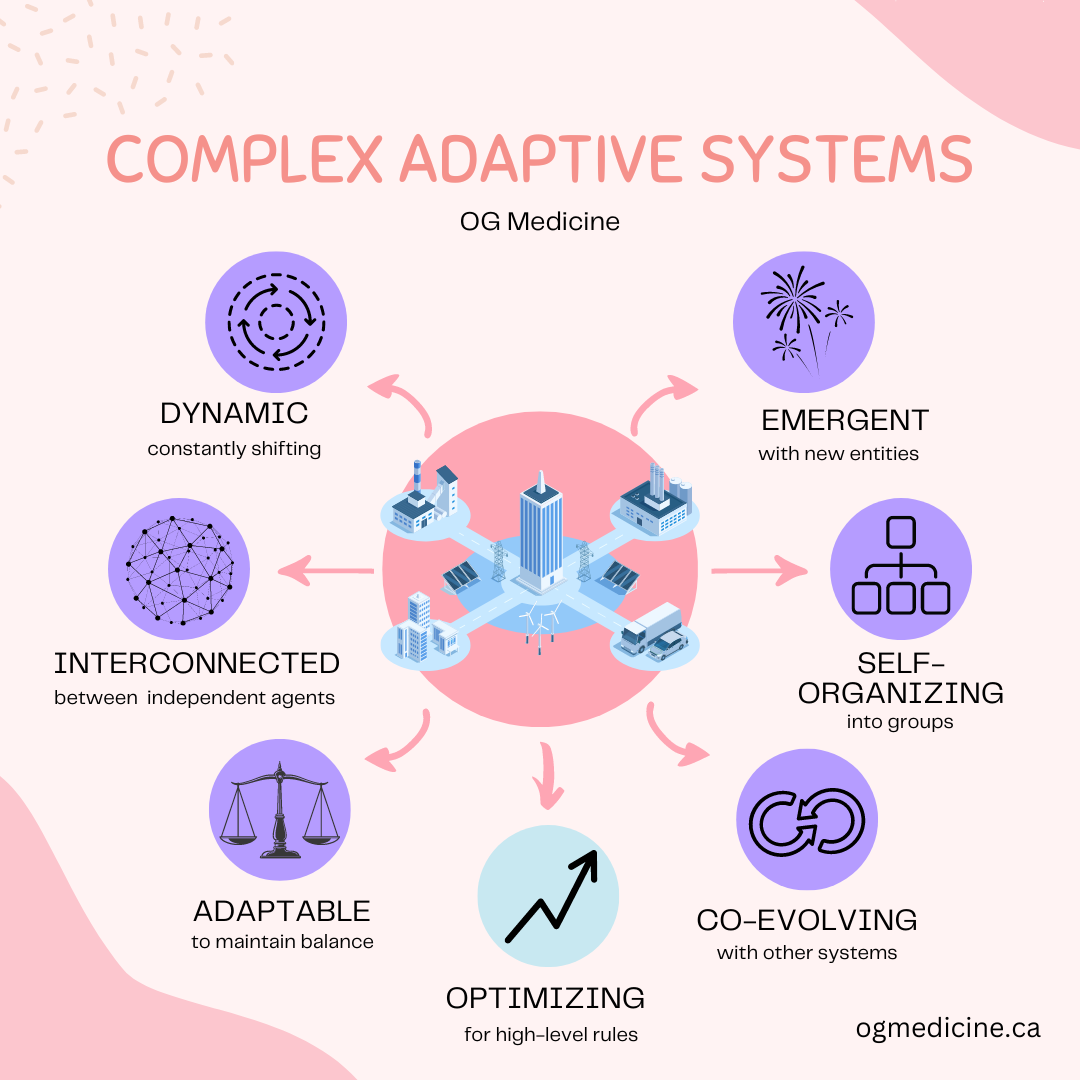
Complex adaptive systems are dynamic, interconnected networks of diverse and interacting components that exhibit emergent behavior and have the capacity to self-organize and adapt in response to changes in their environment.
Huh?
Let’s dig a little deeper.
Key attributes of complex adaptive systems (CAS) that explain why they behave the way that they do.
Complex adaptive systems are constantly changing (dynamic). Think of the stock market. You wake up every day and when the market opens, it starts to shift and change all day-long, as people (independent yet interconnected agents) make buying and selling decisions. How it looks in the morning may be very different than how it looks at night. Due to this dynamism from independent/autonomous agents, you can’t always predict what will happen next (if you can predict the stock market, head to Wall Street immediately).
Yet, the reason for this dynamism is not what you might expect. The constant shifts and pivots you see in the system are actually occurring so as to maintain a balance, or homeostasis, of the overall system. It is adapting to what’s going on in and around it, so as to remain stable. The more flexible and agile the system, the more it can adjust its micro-movements and maintain this fine balance of equilibrium.
Think of the human body - we maintain a delicate balance or homeostasis of an internal temperature of 37 degrees celsius. If our external environment changes (i.e. we are trapped outside in the cold), our internal environment shifts to try and maintain our set point (you shiver, jump up and down, look for shelter, etc).
Taking this one step further, if these external / surrounding conditions persist, you end up with co-evolution of the systems. This allows both to remain “stable”, yet grow. Think of how a prey adapts to predators by evolving new survival mechanisms, but over time the predator also evolves attributes to counter these survival techniques. A plant develops toxins yet the herbivore develops toxin-killing enzymes; and the process continues.
This co-evolution results in emergence - or the creation of new things in the system that are greater than the sum of their parts. They aren’t simply existing pieces strung together, but something that is melded from these things and takes on new properties that weren’t there before. Think of the human body again - our cells and organs combine to create a person - with a personality, feelings, ideas, and behaviours. If you broke us down into our constituent elements, you wouldn’t find evidence of those things in the cells, but somehow when cells and organs combine, they emerge.
Once enough new things emerge, the system naturally starts to re-organize itself (self-organization) into a new structure, or hierarchy. Consider the self-organization that occurred within medicine as our medical knowledge became more complex. As evidence and research mounted, a single human brain could not hold all that there was to know inside - so we began to self-organize into medical specializations. Now, instead of one physician trying (and failing) to know the entirety of medical knowledge, we have dozens of specialities and sub-specialities; general practice -> internal medicine -> gastroenterology -> hepatology.
Why does all of this happen? Why do complex adaptive systems exist, and why do they behave the way that they do?
Scientists are not entirely sure, but one belief is that this overall process of dynamic, interconnected, adaptable, co-evolution equilibrium, is optimizing for some “high-level” goal. It is shifting to maintain equilibrium and bring into optimal alignment some internal rule or structure. The system achieves stability, progress, and perfection, all at the same time.
In a bee colony, it is thought that all of the CAS actions are optimizing for survival of the queen bee, which itself ensures survival of the colony. The medical profession, as mentioned, is optimizing for efficient knowledge-storage (through specialization), which leads to accurate medical care, health of the patient, and thus, survival as well. It becomes a philosophical debate as to what the ultimate “high-level goal”, or meaning of existence of a CAS might be, and by extension, the meaning of life itself. Is it simply survival of the system, or is it something more?
Importantly, while there may in fact be one “ultimate” high-level goal (survival or otherwise), we can also identify many sub-level goals in the system which can appear, at least on the surface, to be in conflict with one another. For example, our healthcare system seems to optimize for patient satisfaction and health and financial sustainability and economic potential and employment, etc. Sometimes these goals align, but sometimes they are disparate to one another, which creates constant push-and-pull tensions in the system. Yet, it is hard to say that any of them could be removed suddenly without destabilizing the system overall, because they each evolved with and around each other. It’s like removing a heart from a human body - the rest no longer works the same way.
Thus, how all of these sub-level goals interact, influence one another, and become necessary or unnecessary over time, remains a complex mystery. Maybe one day we will be able to map out all of the different components of a CAS, the rules that guide them, and minute-by-minute feedback on how they are shifting and changing… but for now, when we try and examine a CAS, it’s like trying to see and predict the movement of electrons inside an atom using the naked eye.
With this in mind, some might argue that it is not possible to influence or control a CAS, because we simply don’t understand all of the moving parts. With healthcare being a CAS, it follows that one might suggest we cannot control our healthcare system.
And yet…
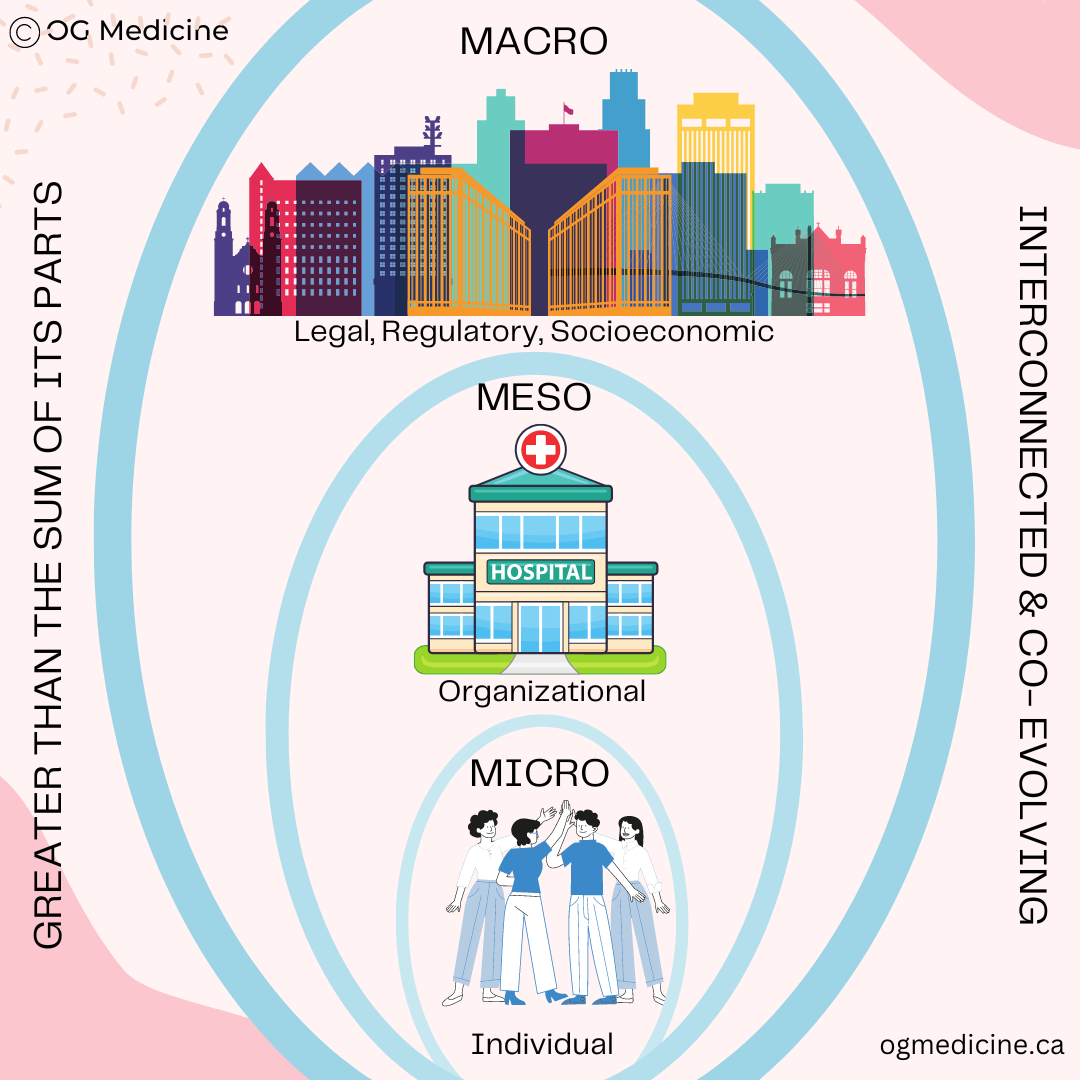
The system begins with the actions of independent, autonomous agents. The micro sets the stage for the macro that emerges.
For this reason, I believe it is possible for us to change the system - we just need to know how to conduct ourselves, so as to surf the dynamic waves of the system, rather than trying to nail down the tide.
What’s more, I believe it is certainly possible for our human actions to destabilize a CAS, and send it into collapse. Global warming, the apocalypse of countless civilizations before us, and the economic collapse of 2008 are just a few examples of how what we do does really matter (the latter of which Meredith Whitney has described as “the feedback loop from hell” (MC Interview, 2023)).
In the remainder of this article, we will look at practical, tangible strategies that we can use at the micro (i.e. individual) level, to influence what occurs in the meso-and-macro (i.e. systems) level around us.
In a previous article I’ve explored the concept of high-level rules in detail, which I encourage you to read another time.
Complex adaptive systems create new things (emergence). These things themselves can become complex adaptive systems. In this way, the micro CAS of individual people exist in a meso CAS of healthcare organizations, which exist in a macro CAS of healthcare systems. Because macro stems from micro, when we change the micro, we can change the world.
PART 3: THE STRATEGY
How to solve problems in healthcare using complexity
There are lots of creative ways to use complexity thinking in healthcare. We’ll cover 3 practical strategic principles below, distilled from evidence and experience. Future articles will continue to explore strategic concepts, so make sure you subscribe to OG medicine.
The 3 principles for today are:
Feedback loops
80/20 Principle
Effectual logic
1) Feedback Loops
Use negative feedback loops to eliminate problems
Feedback loops are central to maintaining homeostasis, and thus wield incredible power in our quest to influence the dynamic adaptation, co-evolution, and optimization of the healthcare system. “Like begets like”, “the rich get richer”, and “the poor get poorer”, are just some of the literary ways of describing the process.
Let’s unpack this further using an example our healthcare minds enjoy - endocrinology.
As mentioned, the human body is also a complex adaptive system, and therefore the feedback loops that our bodies use to optimize the system while maintaining homeostasis are excellent case studies of how feedback loops can work on the larger scale. Analogies are a powerful way to understand complex topics… like complexity.
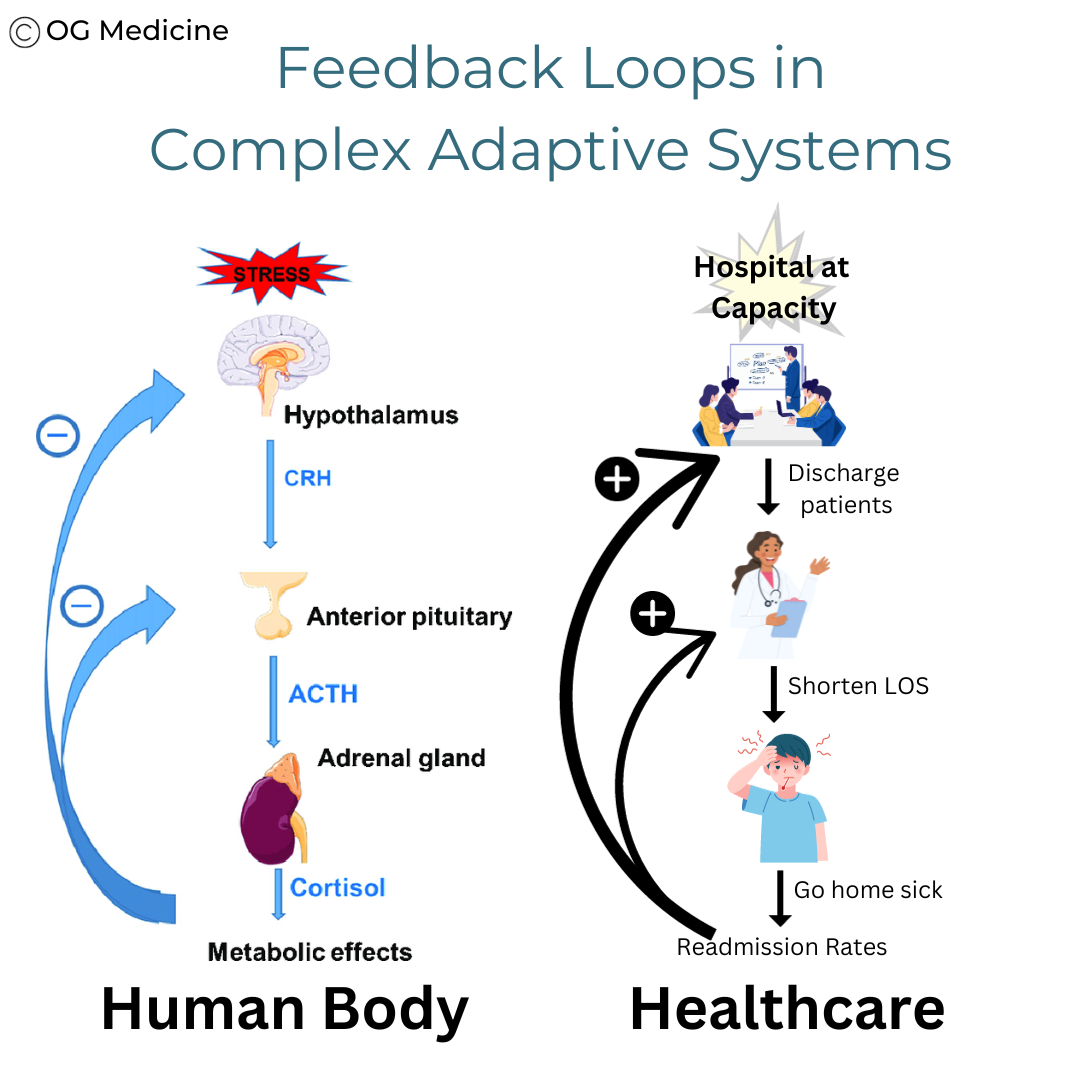
The human body and healthcare system both use feedback loops to direct the system.
Negative feedback loops
In the example shown above, the body’s feedback mechanism for cortisol ensures that we can respond to new, external events/stressors, and maintain system balance to stay alive.
The hypothalamus releases CRH, which signals to the pituitary to release ACTH, which signs to the adrenal gland to release cortisol, which has a host of effects on the immune system, gut, arteries, etc. Because cortisol is able to effectively solve the initial stressor, when levels of cortisol rise it feeds back on the pituitary and hypothalamus to let them know the message was received and the mission accomplished. This results in lowering levels of CRH and ACTH so that the levels of cortisol in the body don’t spiral out of control.
This is an example of a negative feedback loop that keeps the system in balance, while simultaneously solving the problem.
Positive feedback loops
In comparison, the example above also shows a common positive feedback loop in healthcare.
The stressor is a hospital at maximum capacity, to which administrators respond by sending the signal to doctors to discharge patients from hospital more quickly. This results in some patients going home sooner than they should have, and as a result they actually return to hospital not too long after (high readmission rates). This results in worsening bed capacity issues, and actually intensifies the signal coming from administrators.
This is an example of a positive feedback loop, that can quickly spiral out of control.
Strategic Plan: Build More Negative Feedback Loops
Distinguishing between positive and negative feedback loops is of absolute importance when trying to influence a system. This can be summed up by the following two rules:
If you want to reduce something, you need to build a negative feedback loop.
If you want to boost something, you need to build a positive feedback loop **BUT you also need a way of eventually turning it off, or else you risk destabilizing the system.
Prof. Harvey Maylor - business consultant and professor at Oxford’s Saïd Business School - mentioned during a lecture at Oxford that it was very hard to find examples of negative feedback loops in healthcare. I believe this is the root of many of our problems.
Negative feedback loops ensure balance and stability is maintained despite constant external stressors. They are self-healing and self-maintaining.
Positive feedback loops are self-perpetuating, and will continue to build and build and build unless you have some way of turning them off.
I contend that we should focus on building negative feedback loops in healthcare because we don’t have the mechanisms in place to turn off positive loops quickly (although in the future, with Learning Health Systems, we might get close to this).
Again, if we look to the human body - an expert CAS able to maintain system balance while growing from a cell into an adult - the vast majority of its feedback loops are negative. When negative loops are lost (i.e. the pathway no longer functions), you get things like hyperthyroidism, Cushings, frailty, heart failure etc. When we lose negative loops, we get disease.
In comparison, one of the only naturally occurring positive feedback loops in the human body is childbirth. Oxytocin results in more contractions, which results in more oxytocin release, and this keeps going until eventually the baby is born. The pathway then stops not because it’s able to control itself, but because the situation changed entirely - a disruptive event occurred. Without this, it would have continued until the system “breaks” (e.g. uterine rupture).
In healthcare, when we unknowingly create positive feedback loops, our efforts to fix the problem end up creating more of it (push, push push!), rather than maintaining a sustainable system.
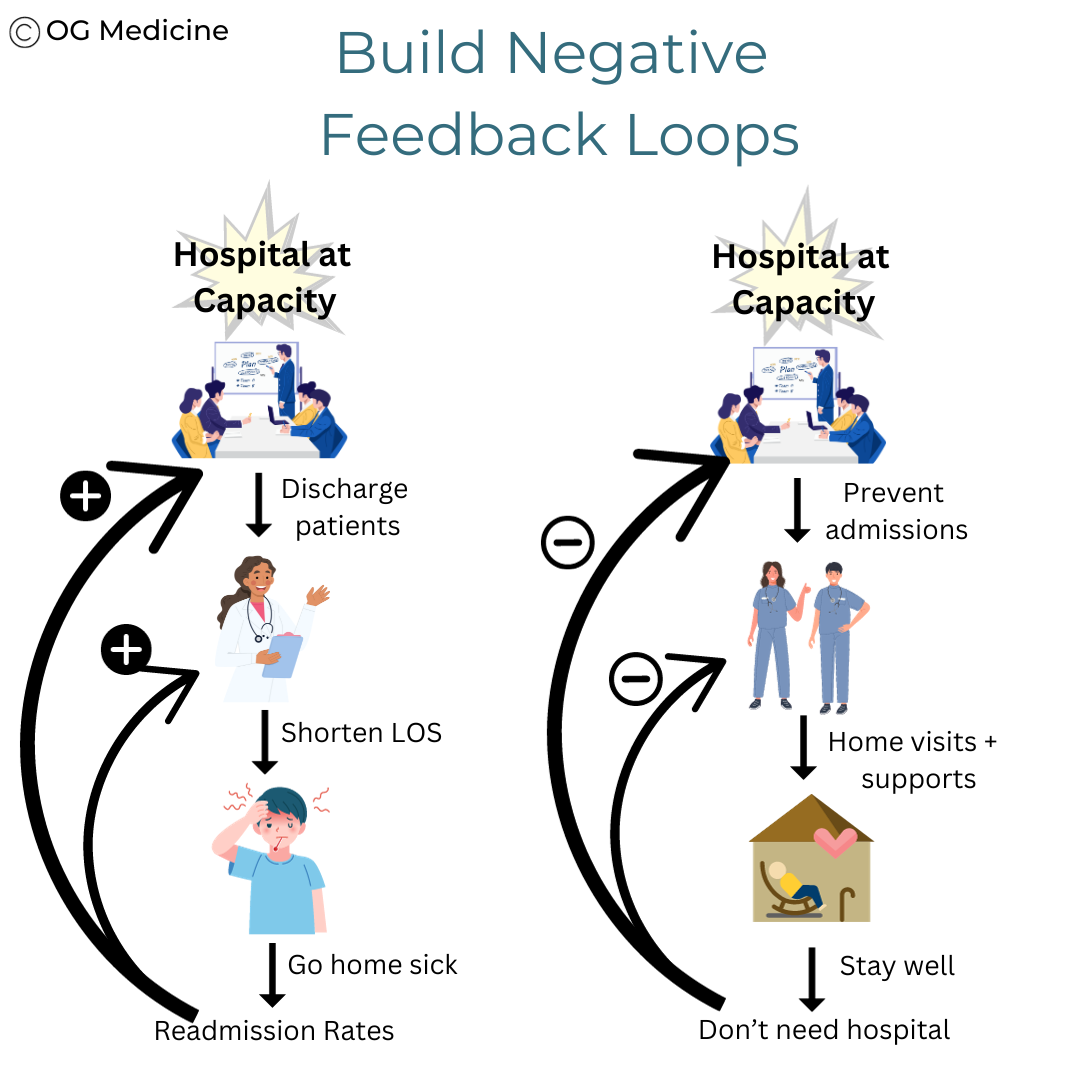
You can see this in the first example above. What would happen if we found a way to solve hospital capacity by turning this positive feedback loop into a negative one?
Many feedback loops in healthcare are positive - meaning that they actually continue to worsen the initial situation that triggered the cascade (i.e. they are self-perpetuating). We need to build negative loops - where the end result of the cascade solves the initial trigger, thus feeding back on the system to shut down the cascade.
Rather than being reactionary to the problem, a negative feedback loop gets at the root cause.
Ask yourself - why are so many people being admitted to hospital? In simple terms, too many people are becoming sicker than what can be managed at home. One negative feedback loop-solution might be to have doctors make home-visits and increase home-care supports, so that people can be kept well at home and avoid hospital entirely. Taking this one (or several) root-cause-step further back, you could even prevent sickness in the first place by increasing diet, exercise, and emotional health resources.
Negative feedback loops explain why prevention is one of the best mechanisms we have in healthcare to ultimately solve problems before they happen.
Let’s walk through another example that demonstrates the thought process behind building negative loops.
How to Build Better Loops
To find effective loops, you need to get to the root of the issue. As they would say in start-up culture - you need to first understand the problem before designing the solution.
Let’s work through an example of trying to increase compassionate care.
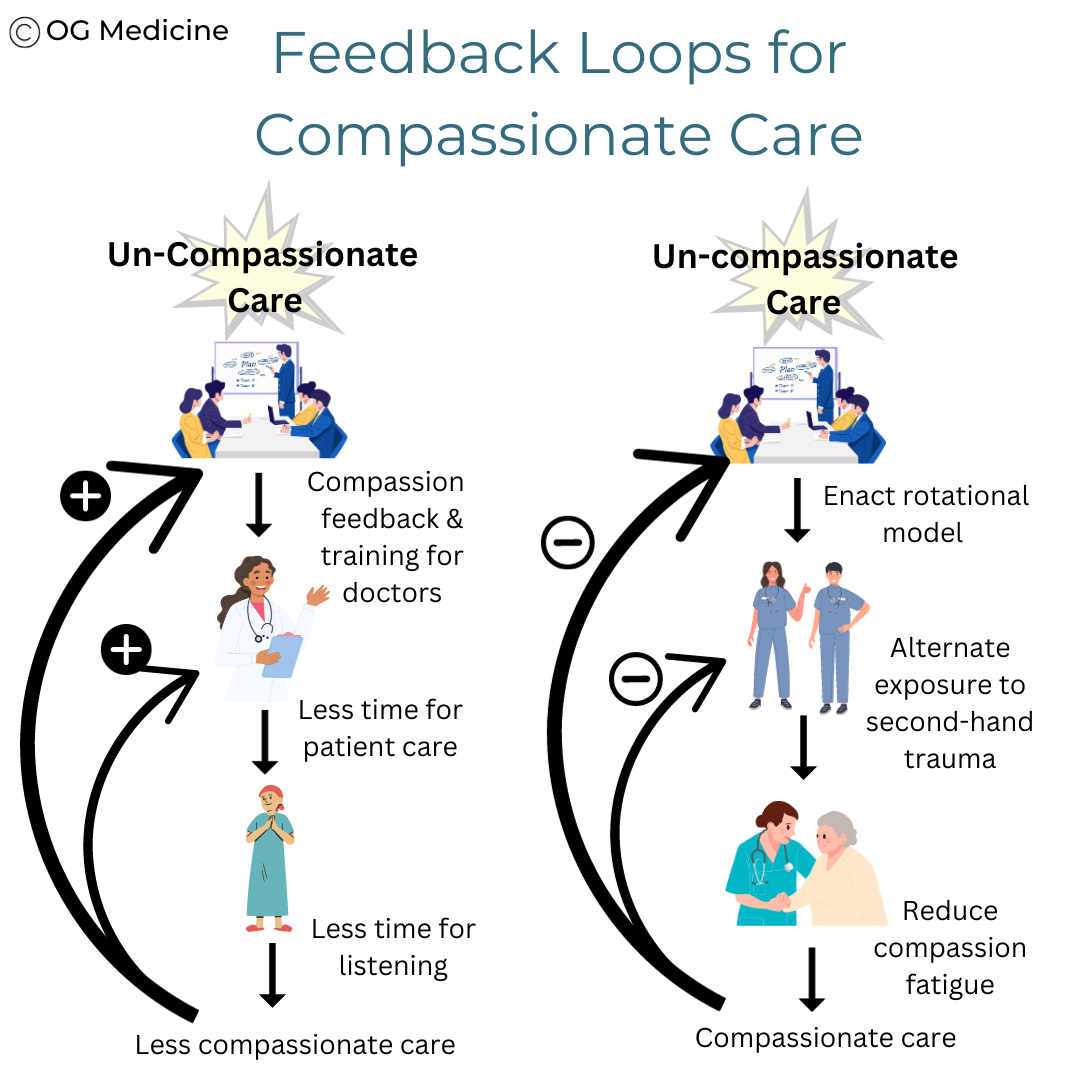
A recent scoping review in 2022 found interventions to improve compassionate care typically involve education and verbal feedback to clinicians (Malenfant et al, 2022). For example, in one study in the NHS the intervention was a “programme focused on supporting compassionate care practice by enabling NHS staff to listen, learn and respond to feedback enabling the development of practice.” (Smith, 2017). These interventions were noted by the healthcare workers in the study to need protected time away from clinical work, “as they need time to plan, undertake, reflect upon and initiate development”.
Yet, this very same review by Malenfant et al identified a key component of compassionate care as having the “availability of time” (Malenfant et al, 2022). The authors did not directly comment on the contradiction between the necessary components for compassionate care and the erosion of said components by interventions used to target it.
This is a classic example of how interventions in healthcare can make things worse when they address a component of a problem rather than the root cause, creating a positive feedback loop for the very thing they seek to eliminate.
Two hypothetical loops for solving compassionate care in healthcare.
Instead, to create a negative loop, get to the root of the problem by asking why.
Why would doctors not be compassionate? Most people go into healthcare with the intention to help others. When they aren’t behaving as such, there is often a very legitimate reason (i.e. every behaviour has a causal reason, a topic for a future article). It turns out, the problem is not that there is too much un-compassionate care; the problem is that there is too much compassion fatigue.
Compassion fatigue leads to un-compassionate care. Compassion fatigue itself is linked to unprocessed second-hand trauma from caring for others and witnessing suffering in high volumes (Canadian Medical Association, 2020).
Therefore, a potential solution is to create a rotational model for high-stress/traumatic clinical services. Nurses and doctors should alternate between highly-traumatic and less-traumatic clinical care. This will provide periods of time without exposure to extreme trauma, lowering emotional exhaustion and thus compassion fatigue, which results in increased compassionate care when back on those highly-traumatic services.
You may notice that this is actually what has naturally occurred in many services - ICU physicians do one week on followed by several weeks off. However, in some medical fields, rotational models might only be necessary in periods of extreme stress - for example during pandemics like COVID-19.
However, a practical requirement to intentionally using these feedback loops to build flexible and resilient systems is the ability to sense signals of early distress - i.e. being able to measure both quantitative and qualitative metrics (e.g. KPI (key performance indictors)), to detect when the desired outcome is drifting from the target. Learning health systems are attempting to close this gap between signal and intervention loop.
In summary, to reduce a problem you need to 1) clearly understand the cause and 2) build a negative feedback loop to reduce it and 3) be able to detect when the problem is over a certain acceptable threshold.
But what if you find a number of different root causes for one problem? How do you decide which one to tackle first?
The answer is to use the 80/20 rule.
2) 80/20 Rule
Solve the 20% of causes that account for 80% of the problem
You won’t find the 80/20 rule formally described in most other resources on CAS in healthcare. That’s because it’s a concept that was developed outside of the CAS cannon, by economist Vilfredo Pareto (and it’s also known as the Pareto Principle).
However, despite the different philosophical origin, the 80/20 rule is an excellent way to operationalize the CAS concept of “non-linearity”, or the principle that small changes can have large effects due to the interconnectedness of the system (Plsek, 2003).
The 80/20 rule states:
20% of the things you do account for 80% of your results
80% of what you do only contributes 20% to your desired goal.
Or, in other words, 80% of what you do doesn’t matter (that much).
This is freeing, because it means we can stop doing 80% of the things we’re doing, and instead, focus on the 20% that actually matters.
This rule exists across nature. it isn’t always exactly 80/20; sometimes it might be 99/1, or 90/10. If you want to read more about the rule itself, check out this book.
However, even without reading the book, the rule makes intuitive sense - we all understand the concept of prioritizing a list of tasks based on what is most important. Another word for this is triage.
The example below shows you how multiple things can be identified as contributing factors to a problem, but not all of them matter that much. If you fail to make this distinction, you’ll spend a lot of time trying to solve aspects that will only make a small dent in the problem.
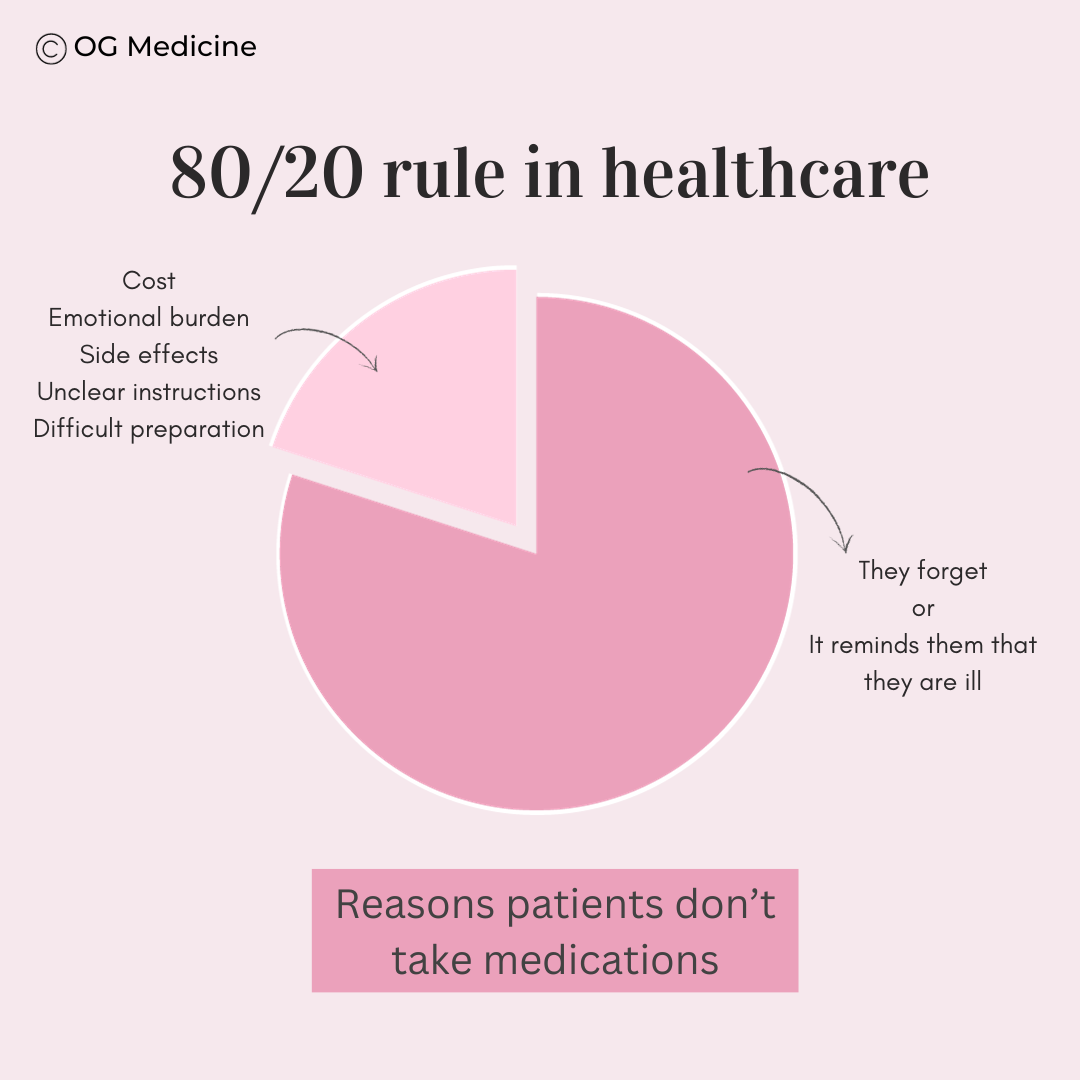
There are many reasons why patients don’t take their medications. The above factors come from extensive research on barriers to medication management. However, only a few contributors actually account for the majority of the problem.
If you tried to solve all of the barriers listed in the article, you’d soon find that no single product or service could achieve this task in a cost-effective and manageable way. It would simply be too complex.
However, if you focus your time and resources on the few things (20%) that account for most (80%) of the problem, you can build a solution that is feasible and effective for the vast majority.
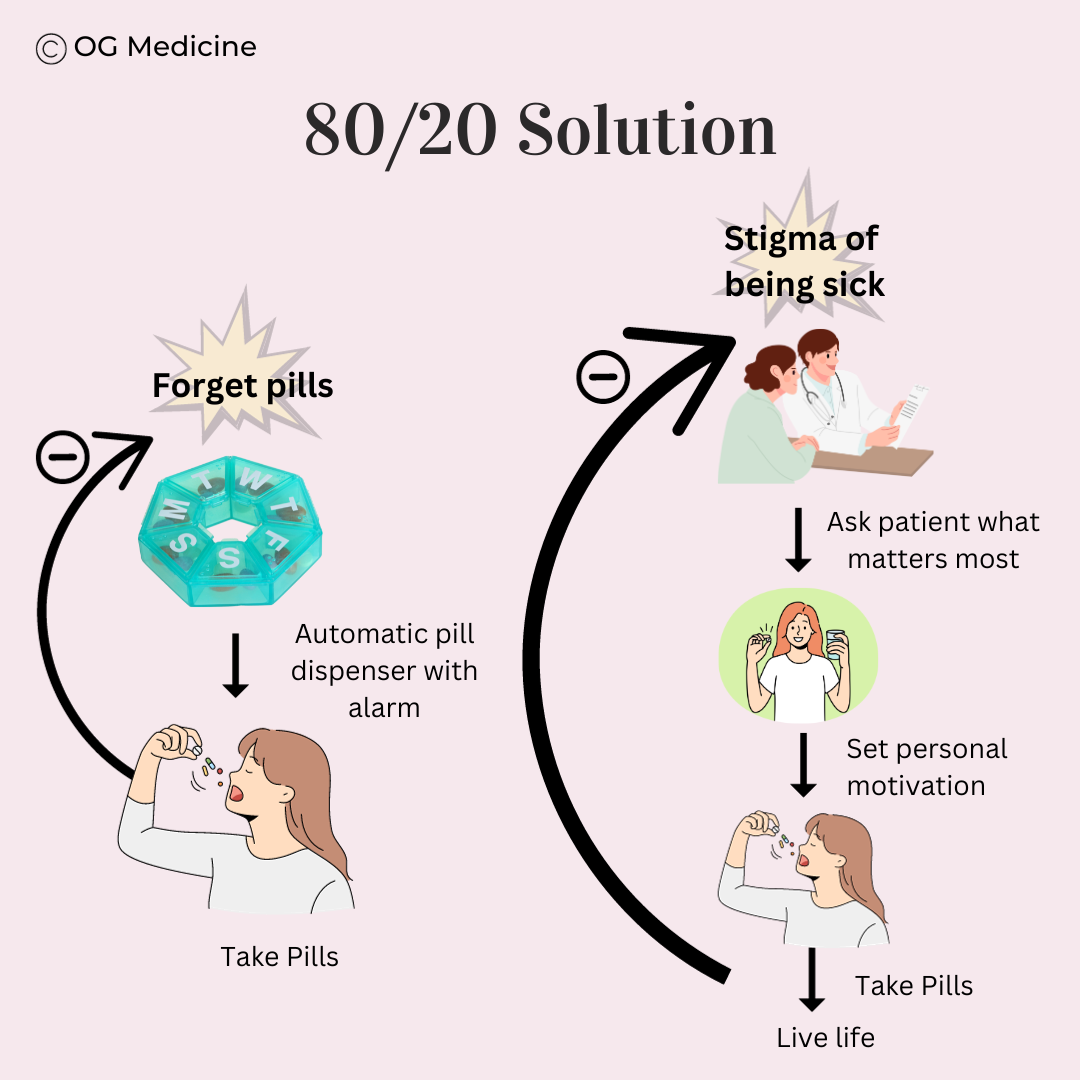
All you need is a reminder system (a negative loop that reduces forgetfulness), and some good marketing/user-design to rebrand the concept of medications from something that focuses on being sick (and induces stigma) to something that enables you to be who you want - you aren’t taking your “heart medication”, you’re taking your “play with the kids pill” (creating a negative loop for stigma).
The intuitive solution to forgetfulness and stigma can be laid out as feedback loops. Importantly, feedback loops don’t always have to be multi-step, as in the case of a simple issue like forgetfullness.
Whether they realize the theoretical mechanism they’re using or not, pharmaceutical industries have understood this well. Have you ever noticed how their commercials feature smiling happy people climbing mountains or playing with their grandkids?
Why is 80/20 so effective?
There’s the logical realization that life is much simpler if you only focus on what matters most. You don’t need to solve every problem. Just the ones that are most important.
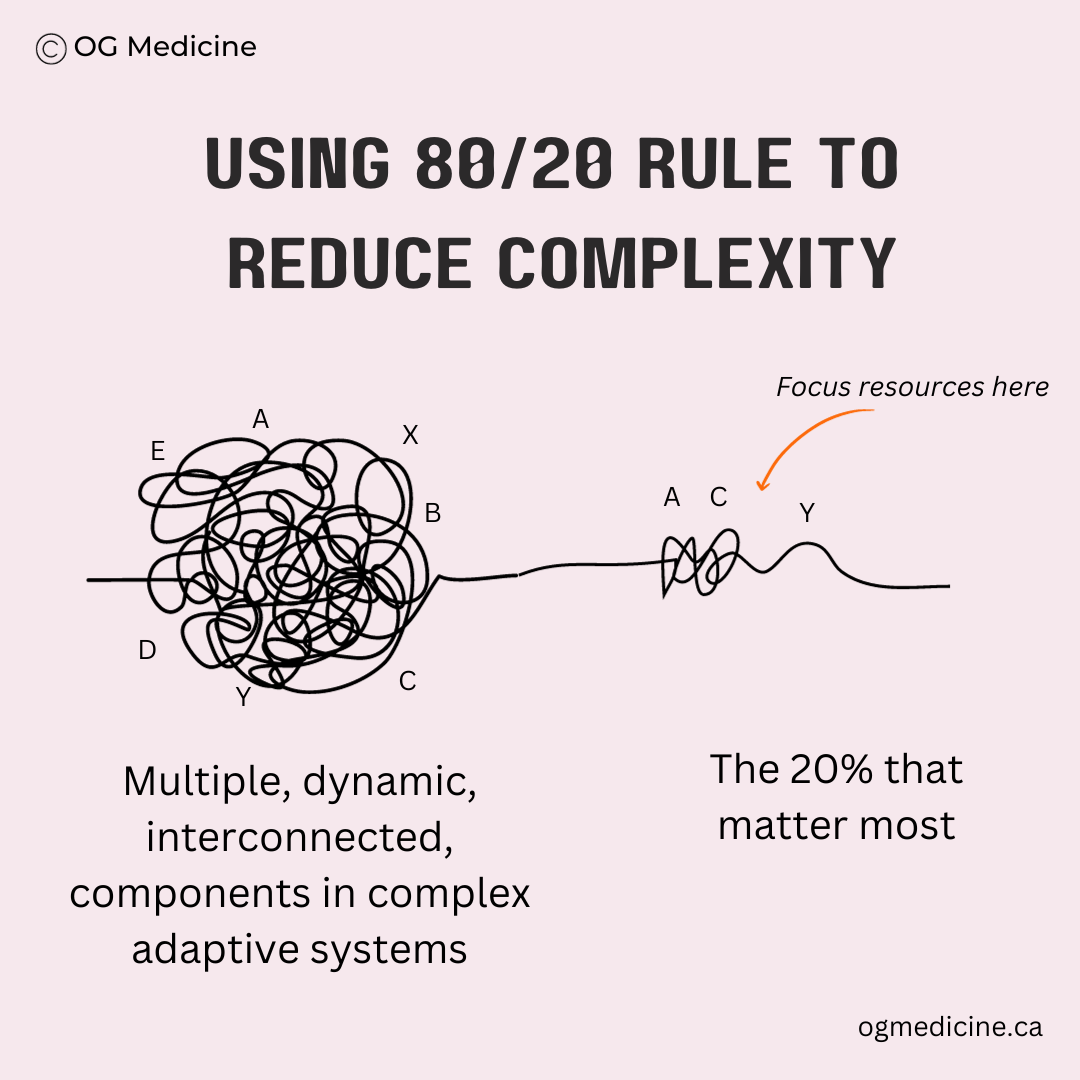
There’s also a deeper reason why 80/20 works - it’s a way to decrease the complexity within a messy complex adaptive system.
As we’ve discussed, CAS are tangled knots of dynamic, interacting components that self-organize into feedback loops that weave in, out and between each other, constantly adapting and co-evolving with the others. This is known in policy systems-thinking as “wicked” problems.
To solve wicked problems you need to reduce the complexity, but you must do so in a way that doesn’t over-simplify the wrong things. For example, a common way of managing complexity currently is to go for the things that are “low-hanging fruit” - simple things that can be immediately solved. But if they don’t have that big of an impact, who cares?
Instead, when simplifying, make sure you are simplifying to the 20% of things that account for 80% of the problem. When you mitigate complexity in this way, you are pulling from theory-based concepts of non-linearity, using the intuitive and practical approach of the 80/20 rule.
Consequences of 80/20
An inherent consequence of the 80/20 rule is that there will be 20% of the problem that you simply ignore. This doesn’t seem fair for the 20% of patients who fall into that group.
It serves the majority, rather than everyone, which is not a long-term solution. Equity is paramount in healthcare. This is a sticky and morally disquieting issue for which I do not have an immediate, all encompassing answer.
However, in reflecting and thinking deeply on this tension (refusing to believe that all tensions cannot be mediated, despite ample evidence in the world to the contrary), I came across an interesting example of how applying the 80/20 rule across different spheres of life might actually help to rectify disparities.
If we were to solve for a seemingly non-patient centered problem in healthcare - cost - the 20% of patients that account for 80% of costs are often part of the 80% of society who receive only 20% of the socioeconomic resources (i.e. are of lower socioeconomic status). In other words, those that are poorest often end up with the worst health, and in later years this results in some of the highest healthcare usage (when care can be accessed).
What this means is that in one realm, these individuals are unfairly left behind by the 80/20 rule, yet if we use that same 80/20 rule to make decisions in a different sphere, we can actually begin to rectify some of this societal disparity. In other words, everyone is in the top 20% somewhere, and applying the 80/20 rule in healthcare has the potential to improve the lives of people who have historically been left behind.
Turning now to even just the most practical of arguments, if you can first knock-off the problems that account for the vast majority of a society’s issues, you have a hope of actually progressing change. 80% better is better than 0% improvement. If you try to solve the problem for everyone all at once, you often subsequently meet impenetrable roadblocks of complexity and cost, which saves no one.
Instead, you can ensure that you continue to cut the 80/20 pie over time. Just because you’re focusing your efforts on the first 20% of things that matter most (right now), when you’re done there will be another 20% of what’s left to focus on. You can keep going in this way, iteratively bitting off more and more of the problem, in a complexity-focused and effective strategy.
Solve the problem by tackling the 20% that accounts for 80% of the problem first… then keep solving the next 20% that matters most until you’ve reduced the problem to an infinitesimally small degree and it is, practically-speaking, solved.
If you’ve made it this far, you now understand how to build negative feedback loops that address the most important 20% root causes of a problem.
But how do you get started if the system is constantly changing beneath your feet?
The answer is to use effectual logic.
3) EFFECTUAL LOGIC
Start with what you’ve got
Ideas in healthcare - even ones that are well-thought-out negative loops with 80/20 principles - have a high chance of failure.
This is because the system is constantly changing, and what you planned may not be what ends up happening. Effectual logic is the secret to how to achieve success in the long-run.
Combining effectual logic - an evidence-based approach - with my experience working as an advisor to healthcare startups, there are three key mantras to remember here:
Success is a moving target
Pivot & Plan
Failure is progress
First, a few words on the science behind effectual logic.
What is Effectual Logic?
Effectual logic is the approach used by successful entrepreneurs to take ideas from garage-room concepts to billion dollar companies that end up changing the world at scale.
I first learned about effectual logic from a classmate of mine at Oxford - a professor at UCL and founder of the Oxford Centre for Entrepreneurship & Innovation.
Believe it or not, entrepreneurship has a HUGE role to play in solving problems in healthcare.
This doesn’t mean we need every solution to be a for-profit company, but we DO need every implementation of a solution to borrow the astronomically successful methods used in other complex adaptive systems, like business and economics.
Think about it. Musk. Bezos. Gates. Jobs. Apart from all being men (*sigh), they are also all entrepreneurs with visions that now influence your life every single day.
Imagine if you could harness that power for healthcare?
Thanks to effectual research pioneered by Saras Sarasvathy and colleagues, we have an idea of the kinds of thought-patterns used by these successful entrepreneurs, termed effectuation.
You can read more about the topic and original work at effectuation.org, but the rest of this article will take effectuation researchers’ key points, put them in the context of healthcare, and explain them as 3 mantras for everyday use.
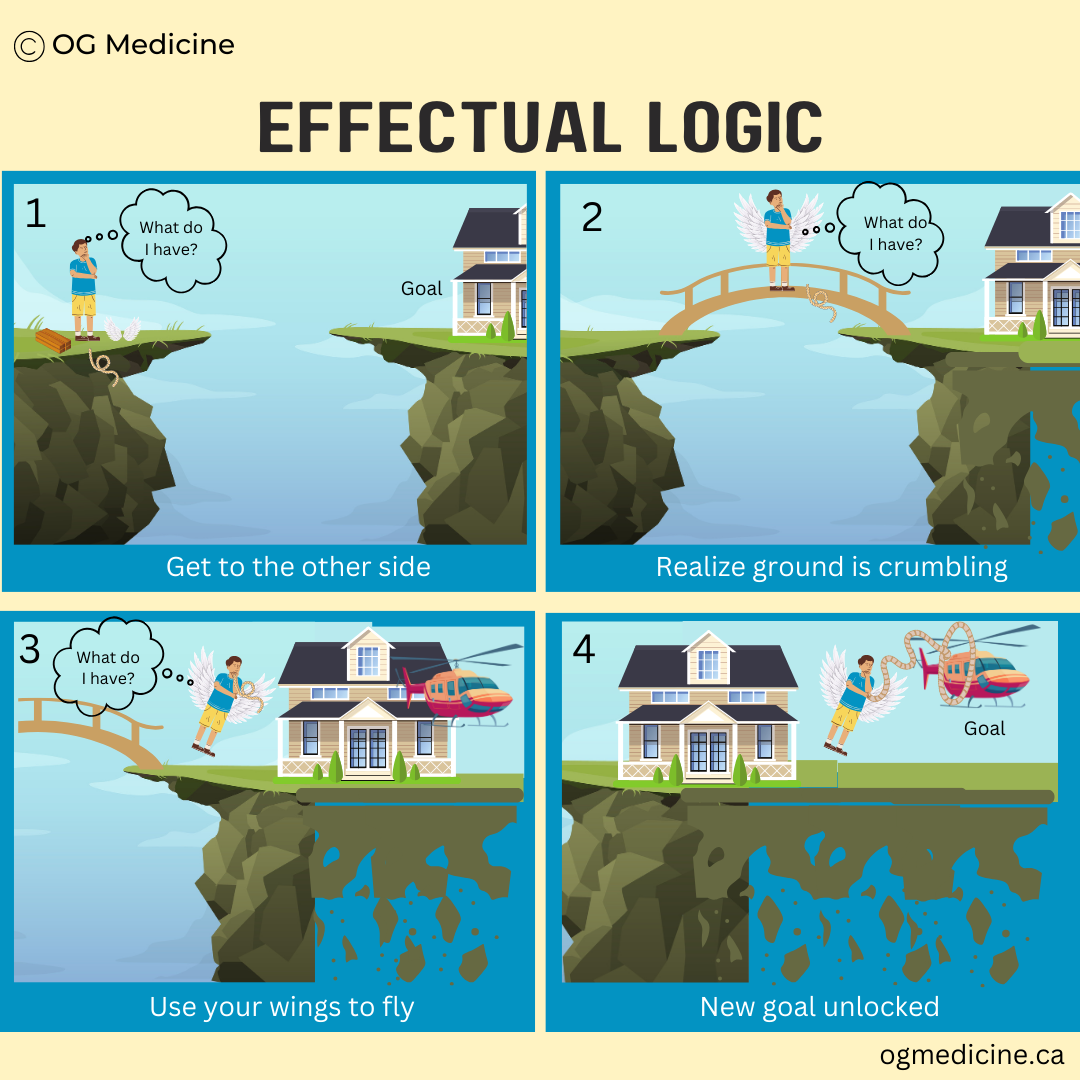
Mantra 1: Success is a Moving Target
We’ve now drilled home ad nauseam that complex adaptive systems like healthcare are unpredictable. You cannot know what is coming next. Everything is uncertain, even when you think it isn’t. Need I reference the pandemic again?
So, what do you do if you can’t predict the future? You stop trying to plan seven steps ahead, and instead you simply make your next move, using what you already have at your disposal.
Be willing to adjust often and rapidly along the way; success is a moving target.
Imagine you’re trying to get to the other side. You think you know what’s over there, but as you go, you realize that the ground beneath the goal is literally crumbling away. You’re able to manage because you’ve focused on what resources you have, rather than what plan you’ve made, and so you can act fast and continue to use what you’ve got to constantly adapt and pivot, rolling (or flying) with the punches.
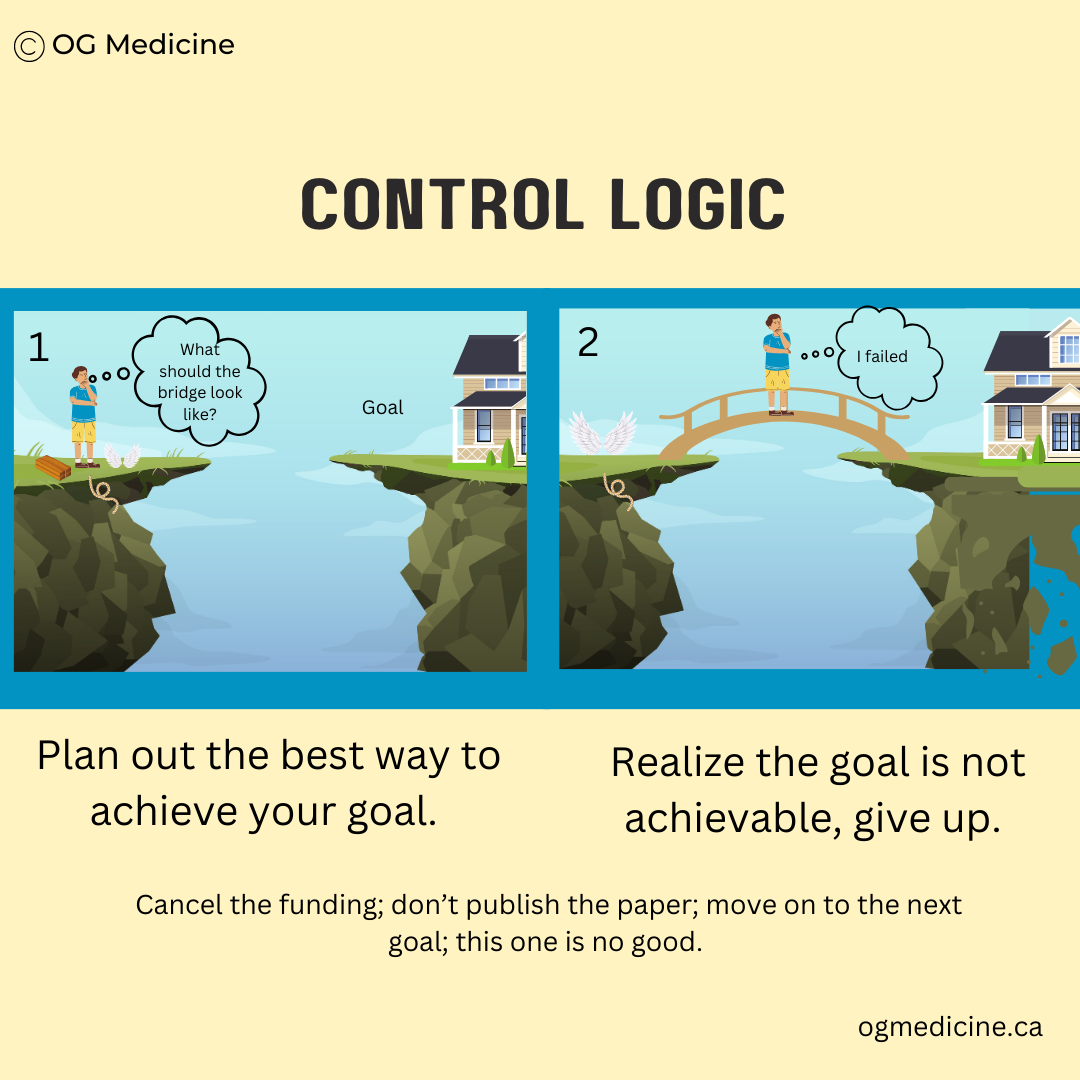
This is the opposite of causal, or what I call control, logic. Control logic is the main mode of thinking taught in many business classes and classic research studies. You’re told to do extensive market research, map the competition, develop a comprehensive go-to-market strategy, etc. Or, in healthcare, engage stakeholders, outline objectives, create detailed plans, apply for funding, etc.
While this kind of thinking CAN be useful (as I’ll talk about in the next point), planning too long and too much does not work in a complex adaptive system where a) you can’t predict (and therefore plan) for everything, and b) things are going to look very different by the time you get there if you spend too much time planning instead of doing.
This relates back to our conversations on the dynamic and adaptable nature of CAS. The longer you wait, the less your plans will apply to what’s going on.
Control (or causal) logic takes a goal and maps out the best way to achieve it. When you’re so focused on your goal and your plan, you see upsets to your ideas as evidence of failure. How many pilot projects are trashed because they didn’t turn out how they were intended? How many millions spent on funding ideas that “fail”? As we will explore, these failures were only the first stage - there was so much more room to grow.
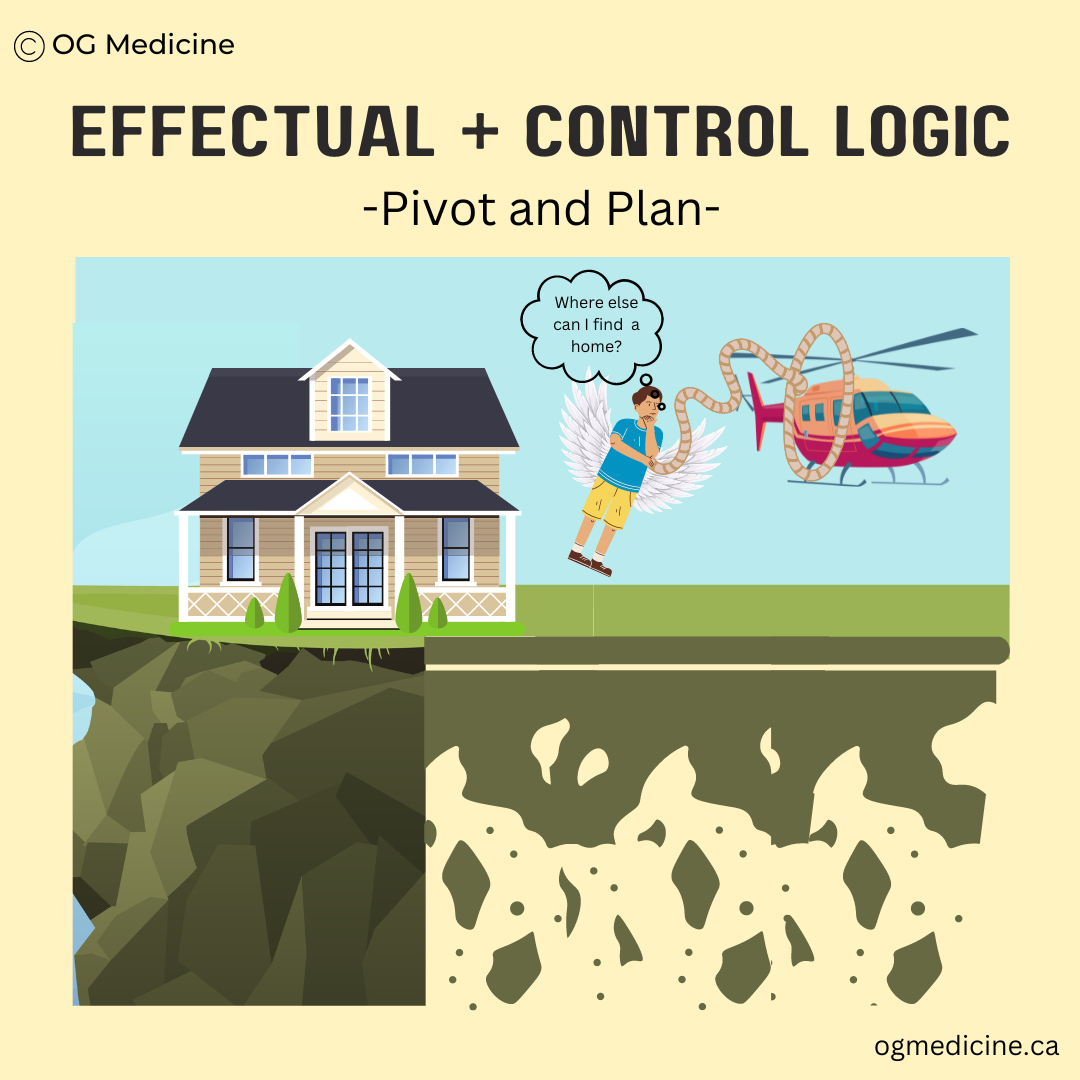
Mantra 2: Pivot and Plan
While effectual logic champions action using existing resources, rather than planning for a distant future, constant pivoting runs the risk of losing sight of what you were initially trying to do.
You don’t want to drift away from your ultimate goal, or vision, and get lost in the jungle.
This is why pivoting should be followed by a brief period of planning, or vice-versa. It is not that control logic is wrong - it’s just not enough on its own.
Both forms of logic are needed for success in the long run.
Control logic will help you keep the goal in mind and inform your immediate next steps; effectual logic will help you survive the complexity and chaos in order to eventually get there.
Even though you have to pivot often in order to ride the waves of unpredictability in healthcare systems, you still need to plan for and keep the ultimate goal in mind. If home (or health) is the goal, you need to continue working towards it, even if the way that you get there looks nothing like what you expected when you started.
Mantra 3: Failure is progress
Think of solving healthcare like playing a video game. You don’t know what’s coming next. You’re going to die a few times before you get to the next level. But you wouldn’t be able to get to the next level without those deaths. You had to gain additional knowledge by attempting different paths, and only then did you learn how to win.
What we see as failure is actually evidence of progress in complex systems - with every “failure”, you’re one step closer to the next level.
One could argue that failure does not even exist. It’s a misinterpretation of the inherent process of evolution in complex adaptive systems. Humanity is in a constant state of evolution and progress. Did humanity fail because we didn’t come out of the primordial soup already having the internet? No. It took thousands of years and many other accomplishments and possibilities, with inherent trial and error, to reach this outcome.
“Evolution and change in large, complex systems comes about through massive testing and pruning of possibilities”
Failure is how the system grows.
However, there is an understandable resistance in healthcare to the concept of “failure”, as it can come with risk to patients. This indoctrinates young physicians and other healthcare workers in a culture of fear towards making mistakes.
Perhaps what we need is to recalibrate our risk tolerance, rather than removing it all together. We can encourage failure on the small things, and focus our “perfectionism” towards things that are likely and catastrophic. Specifically, we can take a page out of the UK’s risk reduction strategy for digital healthcare technologies (see below). Identify sources of risk, mitigate where necessary, and put a full stop to those that are highly likely and catastrophic.
Risk management for clinical safety, used by the National Health Service in England to regulate digital healthcare technologies. For more info, click here.
BONUS
The final (bonus) lesson in the quest to solve healthcare is… there isn’t actually a solution.
Surprise!
While we now know how to solve things in healthcare, healthcare will never be “complete”. There is no solved-steady-state of healthcare out there for us to reach.
What you achieve today will change, if not tomorrow, definitely within the next 10 years, let alone 100’s of future years of human history.
This is because the system will never stop evolving; CAS always continue to change and adapt over time. A CAS may have repeating patterns (hello history), but the echos of the past are always shrouded in something distinctly new.
Thus, the final defining feature of CAS is that progress, or transcendence of the system, is infinite. Continual complex, adaptive, interconnected, and dynamic, where the only certainty is progressive change towards an optimized, stable goal. Just ask existential philosophers, Sarte and Beauvoir.
In Closing
Congratulations, you’ve just completed a crash course in complexity & healthcare change.
To ride the inherent waves of uncertainty and chaos, use the following tools:
Negative feedback loops - define the root cause of the problem & prevent it from happening by turning “off” the trigger
The 80/20 rule - focus on the 20% of things that give you 80% of the results
Effectual logic - remember the 3 mantras: success is a moving target; pivot and plan; and failure is progress.
Good luck and carry on!
Olivia
Dr. Geen is an internist and geriatrician in Canada, working in a tertiary hospital serving over one million people. She also holds a masters in Translational Health Sciences from the University of Oxford, is widely published in over 10 academic journals, and advises digital healthcare startups on problem-solution fit and implementation. For more info, see About.
Influences:
Plsek P. Complexity and the adoption of innovations in health care. National Institute for Health Care Management, 2003.
Plsek P, Greenhalgh T. The challenge of complexity in healthcare. BMJ, 2001;323:625-638.
World Health Organization. To Err is Human: Systems and the effect of complexity on patient care. WHO, 2012.
Khan S, Vandermorris A, Shepherd J, et al. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Services Research, 2018;192:18.
Kannampallil T, Schauer G, Cohen T, et al. Considering complexity in healthcare systems. J Biomed Inform, 2011 (44):6:943-947.
Bucknall T, Hitch D. Connections, communication and collaboration in healthcare’s complex adaptive systems, 2018;7(6):556-559.
Koch R. The 80/20 Principle: the secret to achieving more with less. Crown Currency, 1999.
Greenhalgh T, Abimbola S. The NASSS Framework - a synthesis of multiple theories of technology implementation. Stud Health Technol Inform, 2019;263:193-204.
What is Effectuation. Accessed Nov 2 2023, accessible at https://effectuation.org/effectuation-101#:~:text=Effectual%20logic%20is%20the%20name,world%20view%20and%204%20principles.
Complexity. Bristol Centre for Complexity Sciences. Accessed 2022, available at: http://www.bristol.ac.uk/bccs/about/complexity/